PolicyCore Subscription
Don’t allow your business to fall behind the latest coverage criteria for your product across the payer landscape. The PolicyCore subscription provides real-time email alert notifications and an online portal to access the latest criteria on medical policies. With the PolicyCore Subscription, you can become an expert on how Payers treat and reimburse your therapy, drug or diagnostic test in no time.
Our Policy Email Alerts help you stay alert on the latest changes to medical and pharmaceutical policies across the Payer landscape.

As part of the PolicyCore Subscription, you will receive instant notifications to medical and pharmaceutical policy changes across the payer landscape, tailored specifically to your drug, therapy, and topics of interest.
Our Policy Email Alerts ensures you are notified of any changes that could affect your business, allowing you to act and react quickly.
Our Policy Alerts Include:
- Payer coverage policy changes
- Draft policy changes
- Step-edit updates
- PA Form updates
- Coding updates
- Reimbursement & Billing updates
- Formulary changes (available with a Formulary Viewer Subscription)
Where do you get your data?
Our proprietary, software-driven solution provides the most complete payer coverage dataset on the market. Contact us to learn more.
How can this help my business?
Whether you are a manufacturer, laboratory, provider, pharmacy or other healthcare service provider, the changing coverage landscape can have huge implications on your business. A single policy change could affect coverage for a therapeutic which may increase claim denials, or expand the patient population base. By keeping on top of changing payer policies, restrictions and criteria, you can ensure your patients receive coverage for the therapeutics they need.
Our clients have told us that a single Payer alert on a policy change can save them enough in reduced claim denials to pay for our service many times over. Ask us about other case studies and real-world impact.

How tailored is the information?
We will tailor your subscription so that you receive timely policy updates that affect the drugs, medical devices, laboratory tests or therapies of your choice.
We know you are busy, so we ensure that you only see the information you’re interested in, and prioritizing that information for you is critical.
What’s more, you can schedule your updates so that you receive updates daily, weekly, or any combination of days that suit your workflow.
What will be included in my email updates?
Our email updates are designed to give you exactly the information you need, and a way to learn more if you so wish. Our Payer alerts typically contains the following information for each policy change:
With our PolicyCore Subscription, you can become an expert on how Payers treat and reimburse your therapy in no time. Ask one of our experienced sales team today for a live demonstration of our product suite.
Book a demoAccess years worth of policy updates and payer data, and quickly determine how and when your coverage has changed over time.
You’ll have everything you need to truly understand how the market has received your product or competitor products over time by reviewing historical payer data and changes. Our clients find this information invaluable when predicting future coverage for their product portfolio.
With our database you can search for a broad range of policy updates, or hone your search to a specific Payer, state, date range or more.
Our search filters accommodate a wide range of search criteria, including filters such as:
With our PolicyCore Subscription, you can become an expert on how payers treat and reimburse your therapy in no time. Connect with a member of our team today for a live demonstration of our product suite.
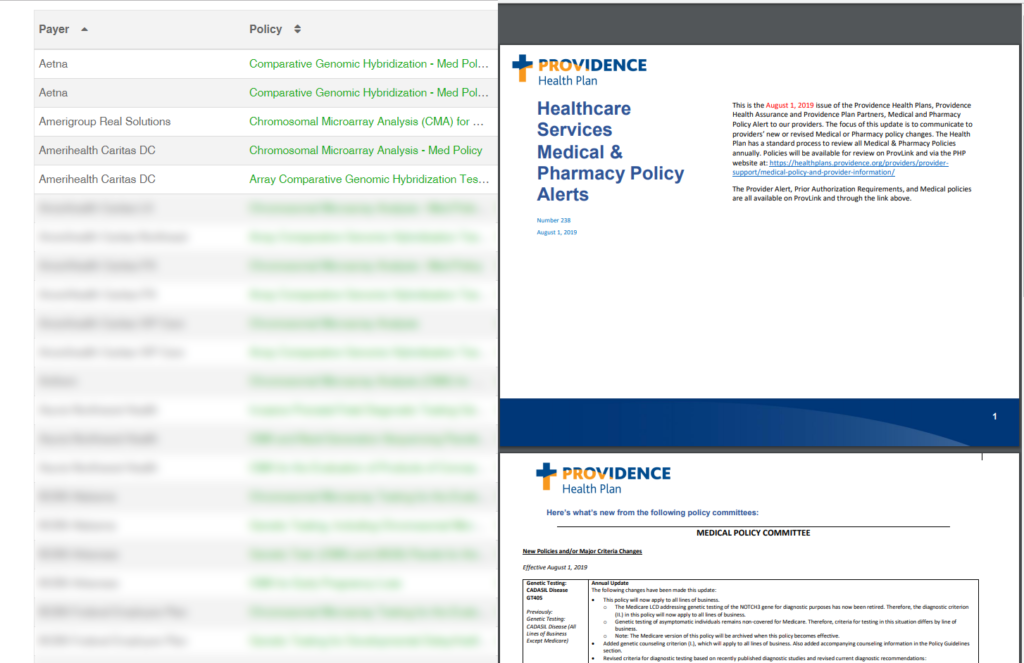
Book DemoIn addition to Historical Policy Database, we host the most complete database of live Payer policies and documents on the market, so you can stay up to date on the latest payer data.
Find the Payer policy documents you need fast using our interactive dashboard. Search by therapy, drug, diagnostic test, payer, state and plan type, to find the desired document(s). We offer a link to that exact document so that you can review the material for yourself.
- Medical Policies
- Pharmaceutical Policies
- PA Forms
- Coding Guidelines
- Provider Manuals
- Fee Schedules
- More..
What’s more, we’ll let you know when a given document was last updated, whether it was a pharmacy benefit or a medical benefit document.

With our PolicyCore Subscription, you can become an expert on how payers treat and reimburse your therapy in no time. Connect with a member of our team today for a live demonstration of our product suite.
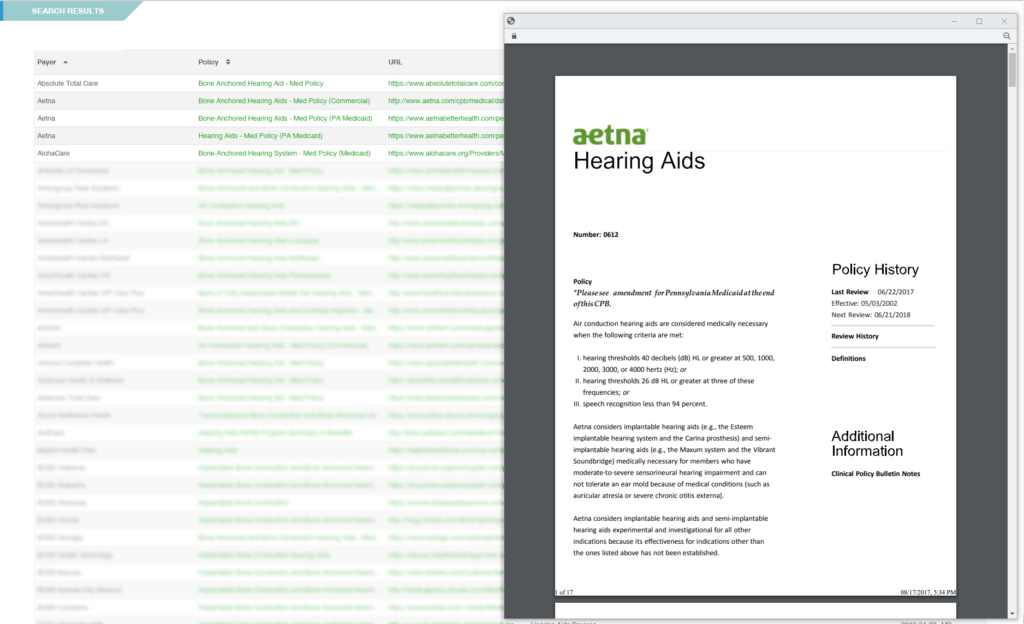
Book DemoQuickly access the exact policy you are seeking with our Advanced Policy Search. Easily pull the exact medical policy you're seeking with our advanced search filters.

Advanced Policy Search provides...
Our universal search function allows you to search down to the most granular level to find the precise policy, form, or coding guideline you are looking for. Whether you are in need of a medical or reimbursement policy, a prior authorization form or a pharmacy policy, Policy Reporter allows you to keep on top of the latest criteria documents in real-time.

With our PolicyCore Subscription, you can become an expert on how payers treat and reimburse your therapy in no time. Connect with a member of our team today for a live demonstration of our product suite.
Book a demo
