Acumen Suite: Market Access Tools
Want to maximize market penetration for your drug, medical device, biologic or diagnostic test? Need expert input in unlocking new markets or Payers? Our market access tools are here to support your business growth plan, highlighting the best course of action to set forth for success.
Our Online Payer Landscape Dashboard revolutionize the way you access and utilize vital policy insights - bringing unparalleled centralization and integration to provide you with a comprehensive and streamlined experience.
What’s Included
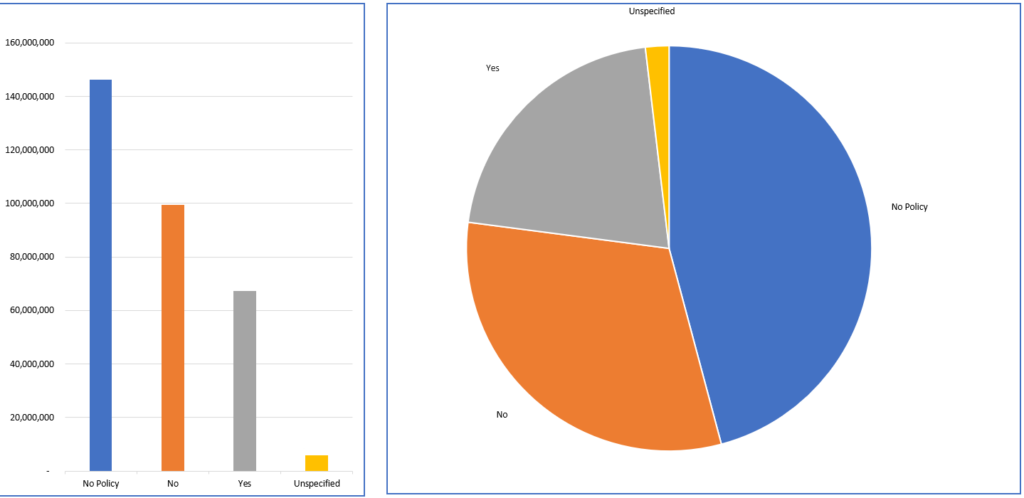
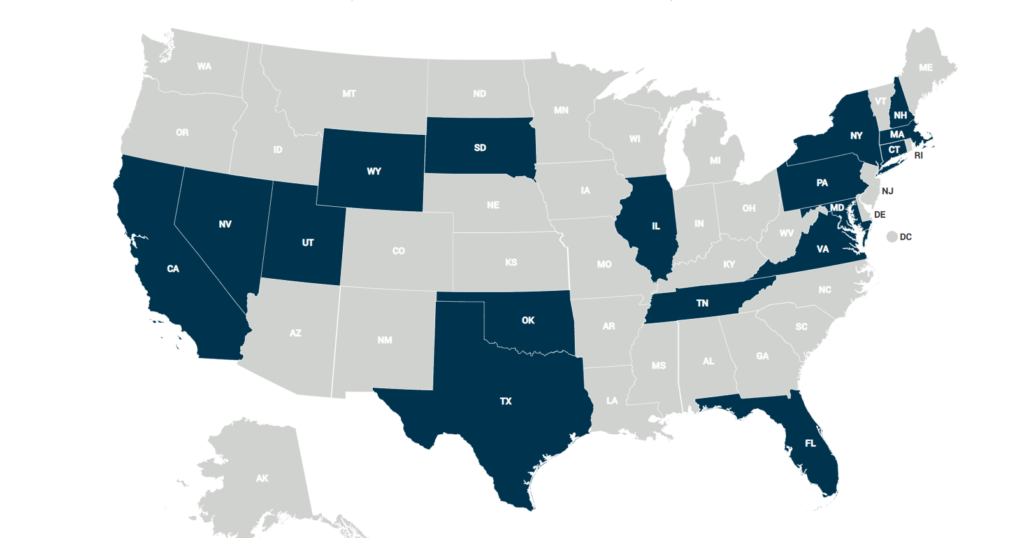
Key payer statistics such as enrollment numbers, plan dynamics, and geographical presence
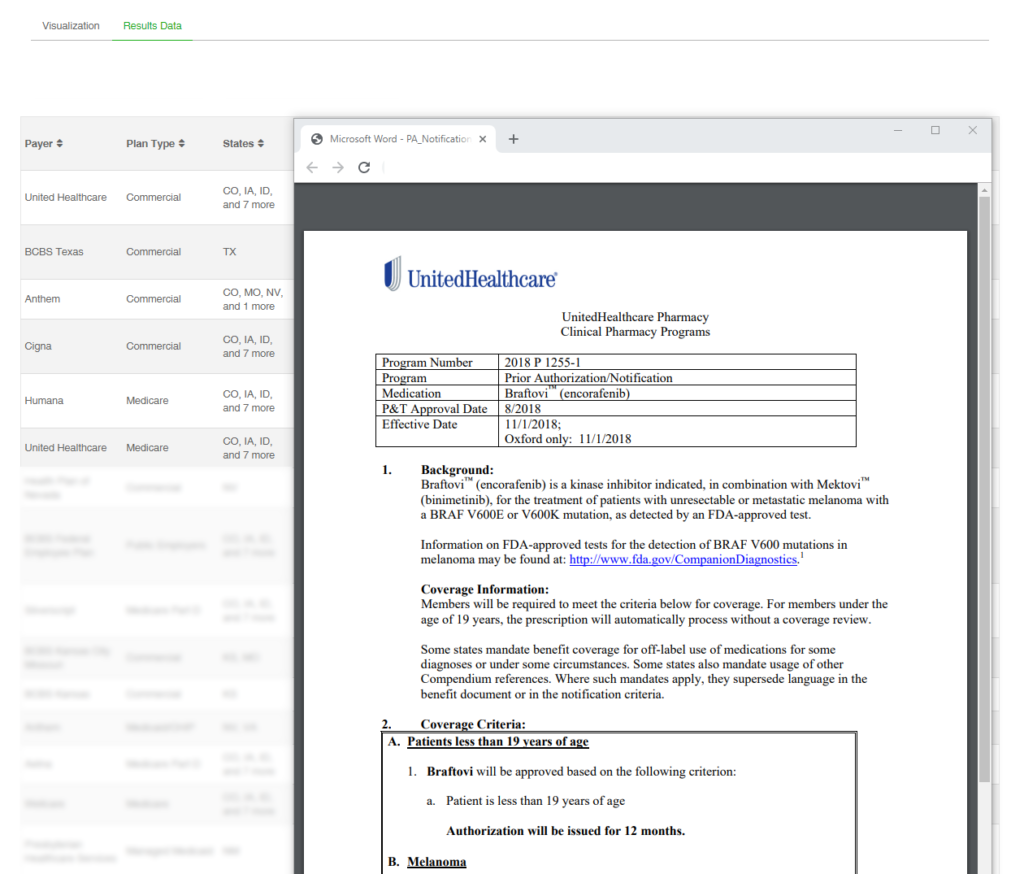
Coverage criteria of your therapy by payer and plan type across all available payers
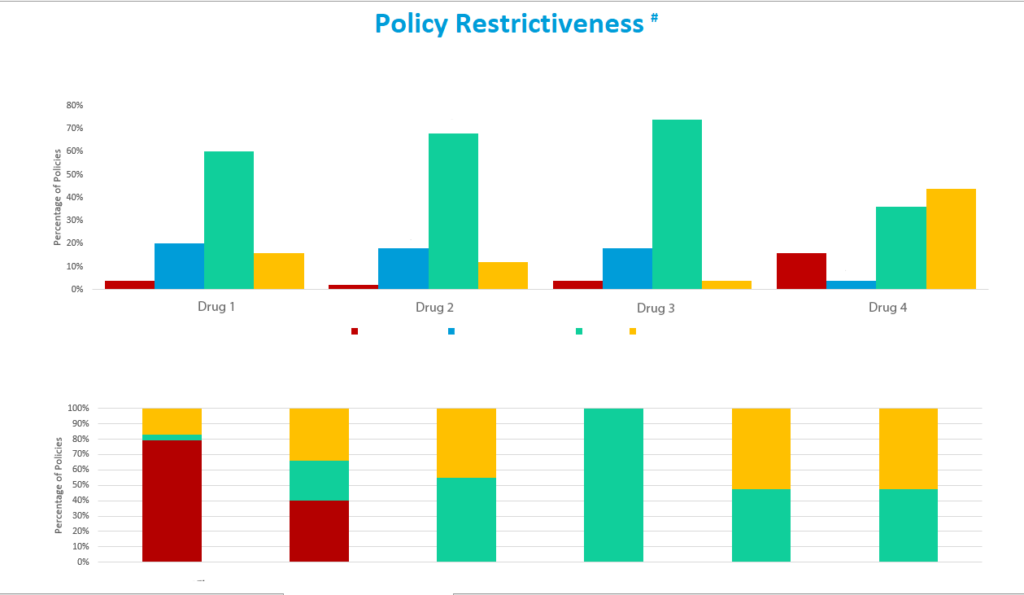
Coverage of competing therapies and a comparative analysis
Key restrictions such as quantity limits, step therapy, and prior authorization, and more
Access to your reports anytime, anywhere through our secure online portal
Interactive dashboards that visually represent key parameters, offering an in-depth understanding of complex therapeutic areas
How Does This Drive Revenue?
Payer Landscape Dashboard Reports provide you with critical data to create, execute, and develop your market access strategy. Allowing you to:
Giving insight into how payers treat your product across the marketplace, including where coverage is strongest, which regions and providers to target, and how to tailor your payer advocacy efforts.
Identifying where coverage exists, where it does not, and where there may be barriers to patient access, allowing you to deploy your sales and marketing strategies effectively and efficiently.
Highlighting not only which Payers cover your drug and how, but which do not, thereby informing an accurate and effective patient, provider, and payer communication strategy.
Have It Your Way
We can facilitate a number of delivery options to suit our client's workflow, including:
Book a demo with one of our experienced sales team today to find out more about how our data can optimize your sales strategies.
Book a demoOur Coverage Viewer tool is a powerful, user-friendly dashboard to learn about your therapeutics coverage criteria across almost all Payers in the U.S.

Common Uses of the Coverage Viewer
Sales and Market Access teams use the Coverage Viewer tool to identify, assess, and optimize patient access for the select therapeutics of interest. It is designed so that each of your account managers can strategically focus their sales efforts, select and view their territories and inform physicians of the latest criteria.
By utilizing the Coverage Viewer, you can quickly view, monitor, and analyze coverage for your therapeutic, as well as alternative therapies, instantly across all 50 states from one place, enabling you to effectively strategize and ensure commercial success.
CV-Rx
Coverage Viewer – Pharmacy Lives
Providing the best in class policy coverage criteria layered with pharmacy covered lives figures.
In addition to Coverage Viewer, CV-Rx combines Policy Coverage Criteria with Pharmacy Covered Lives to be able to assess health plans and PBMs on top of Payers. We report both PBM Covered Lives and PBM Client (health plan) Covered Lives for pharmacy benefit coverage to better differentiate access and coverage criteria.
The data set is configurable to best suit your market access needs.

Informing Your Providers
Our tool enables your team to export either a simplified or detailed summary of coverage criteria for easy access to providers offline.
At each provider meeting, your account manager can bring this summarized report, which highlights coverage for your therapeutic by plan.
Book a demo with one of our experienced sales team today to find out more about how our data can optimize your sales strategies.
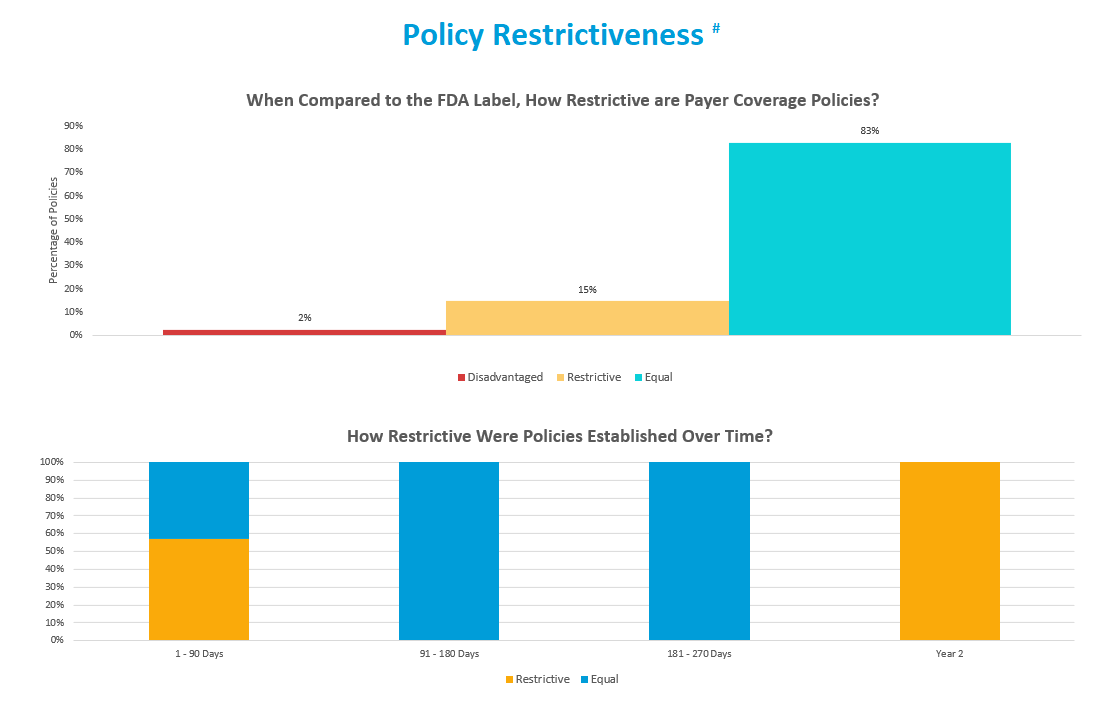
Book a demoUnderstand coverage, restrictions, and criteria before commercialization to know how Payers will treat your product upon launch. Our Predictive Payer Coverage solution assesses the present and future coverage risks facing your brand, and provides strategic insights necessary to help mitigate them.
Solution Process
The solution leverages Policy Reporter’s proprietary data, historical insights, and predictive modeling and combines this with our decades long insider experience to give you a comprehensive forecast of your payer market. We use a data-driven approach to identify key targets and provide tactical recommendations to maximize your coverage.
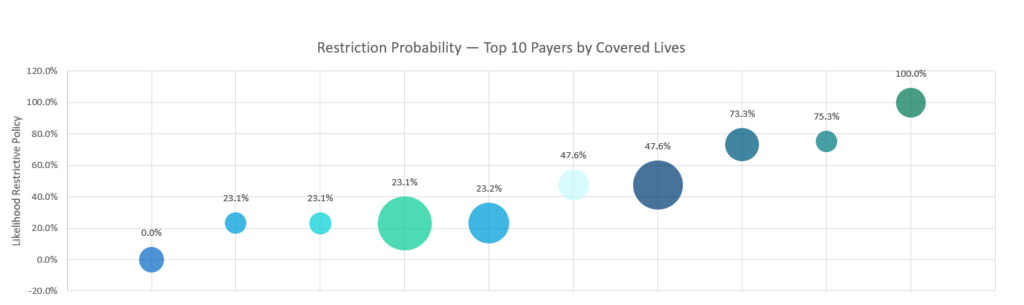
Predictive Modeling
Based on custom reporting, we analyze and predict likely access risk and opportunities your product can face upon launch. We are able to run risk assessments to help clarify your high-priority targets for your post-launch access.
Custom Report
We walk you through a customized, comprehensive report to provide insights into payer trends and most likely access scenarios.
We Answer Your Burning Questions:
- Which payers are most likely to cover?
- What restrictions and criteria are most likely to be in place?
- Are there certain HTAs, studies or guidelines that will influence coverage?
- What is the timeline to policy publication or formulary adoption?
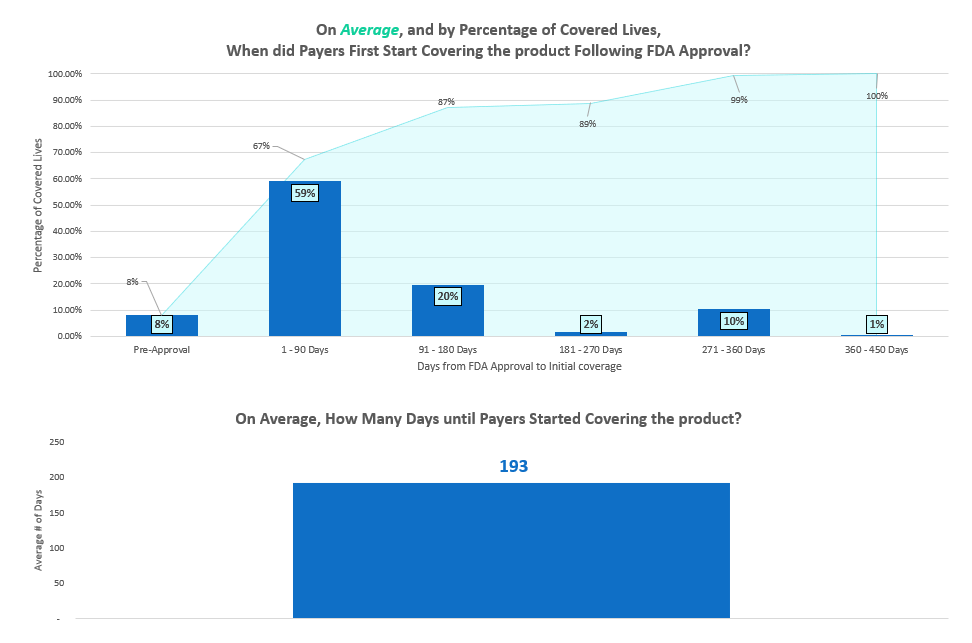
From FDA Approval to Initial Coverage, a Detailed Analysis:
Our custom reports seek to arm you with the knowledge you need to make your product succeed. Our thorough analysis provides:
Predictive Executive Summary & Strategic Recommendations:
We work with you to identify and target payers for monitoring and intervention, allowing you to allocate resources accordingly to contain any potential risks.
We deliver a strategically-oriented plan of action focusing on the lines of business and geographies pertinent to your goals, while identifying the payers of interest that you can engage with in confidence.

Payer Validation
We can provide access to a virtual panel of medical and/or pharmacy directors from a selection of plans to validate the predictive modeling, provide key insights and strategic input into your go-to-market strategies.
Connect with us today to book a consultation and stay ahead of the market.

Book a demo with one of our experienced sales team today to find out more about how our data can optimize your sales strategies.
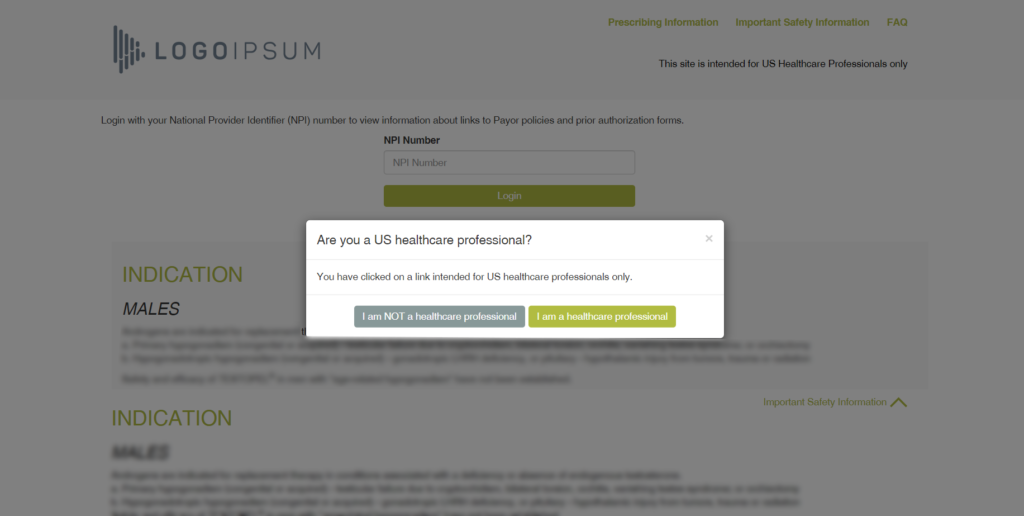
Book a demoThe Patient Access Lookup (PAL) Portal is a powerful tool to help Providers and Patients submit claims. At its core, the PAL Portal facilitates claims submission by helping Physicians and Patients walk through the requirements process.
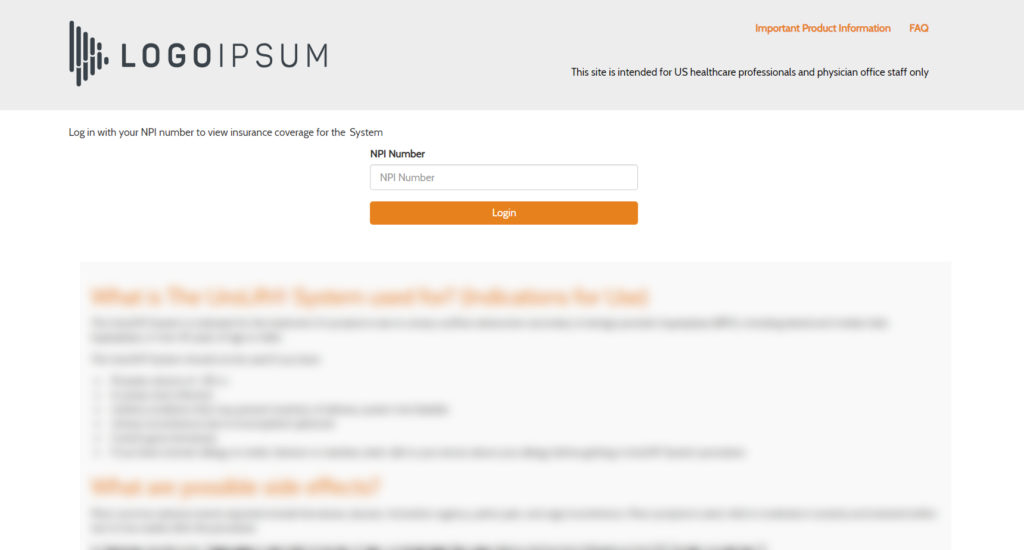
The PAL portal offers Providers and staff a centralized space to easily review relevant documents and information regarding a patient’s coverage, quickly accessible from your own website.
PAL hosts Payer information and its related documents such as prior authorization forms and reimbursement information on specific tests, devices or drugs. PAL was designed with the user in mind, offering you a customizable web portal to match your branding requirements and support your existing workflow. Alternatively, key Payer information can be embedded directly into your existing Provider support website. Talk to a Policy Reporter Technical Specialists today to learn about the options.
PAL helps to reduce claim denials and reduce reimbursement and patient support center calls. It supports the patient’s authorization process and helps patients get on therapy and stay on therapy.
Case Study:
A major pharmaceutical company subscribed to Policy Reporter’s Patient Access Lookup Portal to support a mature product that specific authorization criteria and was on a step edit. At launch, the Portal provided key support for physician’s offices looking to understand patient eligibility and submit claims. Within a matter of weeks, the client was able to shut down their reimbursement hotline, saving the company hundreds of thousands of dollars per year. In addition, providers were receiving fewer claim denials.
Book a demo with one of our experienced sales team today to find out more about how our data can optimize your patient access workflow.
Book a demo
